Plot Twist
- Bill & Amanda Batterson
- May 6, 2020
- 9 min read
This is part three of our little Judah's birth story. You can find part 1 here, and part 2 here.
It was so surreal when we rounded the corner and saw our sweet little babe laying in that bed, hooked up to wires with a team of nurses were standing around him. They explained to us that he had too much fluid in his lungs, which was causing him to work too hard to breathe. It's called Transient Tachypnea (TTN) and is common in c-section babies. When babies travel through the birth canal during a typical delivery, the fluid gets squeezed out of their lungs, but with a c-section, that doesn't happen. Combine that with his size and his prematurity, and it just was a bad combo. They explained that it was a common condition and were very reassuring that everything would be okay, but that he would need to remain in the NICU for a few days until it cleared up.
They would treat him by giving him oxygen through a canula, but they also wanted to put in a g-tube. Since he was having trouble breathing properly, he was also having to work extra hard to nurse. He'd only latched once in the first 12 hours and it didn't last long. So the g-tube would be inserted as a back-up way of feeding him if it came to that, and also as a way to make sure air didn't build up in his stomach as a result of the nasal canula. They also needed to run an IV of fluids and electrolytes so he didn't get dehydrated from not nursing, to make sure he could regulate his blood sugar, and as a way to administer antibiotics if his labs came back showing infection.
After that whole explanation, we gave consent and watched while they inserted the IV and the g-tube. I asked if I could hold him when they were all finished and, with a sad look in her eyes, the nurse said, "I'm sorry, but no. It's best for him to stay in the bed because we need to closely monitor his stats. Once we get things under control you'll be able to hold him, but for now we need to keep him in the bed." That's when the tears came. All I could do was sit

there next to my sweet baby and hold his tiny hand. I couldn't hold him close after the trauma that he'd just been through and that was enough to break this mama's heart. I asked about feeding him and they said they'd call me down as soon as he woke up so I could try to nurse him.
I didn't want to leave the NICU, but he was drifting off to sleep and they said the more he slept, the better it was for his body to be able to work at getting that fluid out of his lungs. So we wheeled back to our room. Our empty, too-quiet, room. With no baby. I hated being away from him. I was exhausted physically, and so sore from surgery that it hurt to cry, but I couldn't stop the tears. I just wanted to hold my sweet boy.
Within a couple hours they called me down to try and nurse him. Before we unwrapped him they needed to check his stats, and they let Bill take his temperature.
It was so sweet to be able to pick him up and hold him, but also so hard with all the wires and tubes to keep track of and try not to get tangled up in. The poor guy was trying so hard to latch and eat, but that g-tube just kept him from getting completely latched to get good suction, and my milk still hadn't come in. It was so hard to not be able to provide him what he needed. The nurse asked if we were willing to try formula, but I really didn't want to head down that road just yet. She reassured us that we could keep putting him to the breast every three hours to help my supply come in. If it still wasn't happening in the next couple of feeds we'd need to sign consent to give him donor milk. So we sat with him a bit longer, not wanting to let him go, but seeing that he was dozing off and needing more sleep, we headed back to the room to consult with the lactation specialist about how to get things flowing.


She showed me how to use the pump, and how to hand express since pumps often weren't the most efficient at getting milk out. I had pumped before with Owen, and it was no big deal, so I wasn't too worried. Little did I know just how grueling it is to eek out a tenth of a milliliter of colostrum to nourish my sweet boy.
The next time in the NICU we tried nursing again, but it wasn't working. So we tried our first bottle of donor milk. It took him a bit to get the hang of the bottle, but once he did, he was one happy baby.

We soon got into a rhythm: As soon as we left the NICU the two-hour clock would start. They wanted him to eat every two hours so they could track his blood sugar regulation and his output. For the first hour back in the room I would try to pump/express milk. Often, only getting drops. There was a whole set up: pump for ten minutes (which achieved nothing, but I had to try) hand express for about 45 minutes, using a plastic spoon to catch the drops of colostrum in, then use a syringe to suck the colostrum from the spoon, then label the syringe with our sticker and the time it was collected. Bill would wash/sanitize all the things afterward. Then I had an hour to rest/nap, eat, get poked, prodded and pushed to move use the bathroom etc., so I could get my own healing going. Before we knew it, it would be time to head back to the NICU to give Judah the minuscule amount of my own milk from the syringe, before giving him the donor milk in a bottle. We'd cuddle and swoon over him as long as possible, before he'd doze off again and the cycle would start all over.
Each time we went to see him we got an update from the nurses. The first couple of days were about the same. Then we started seeing some changes. His oxygen flow was able to be turned down to nearly nothing (meaning he was almost able to breath on his own without stressing his lungs/heart out). and he was slowly but surely filling diapers, which mean the fluid was getting out of his system. Soon, he was well enough to be unhooked from all the wires and tubes long enough to get his first bath. He was so excited to get unhooked from everything. (In fact, they ended up having to use the strongest tape they could just to keep his canula in because he kept reaching up and pulling it out.) He was NOT so excited about bath time. But happy again to be done with bath, put on clothes for the first time (over the wires) and get snuggled with mama without the tubes for a while. The sweet nurse even gave him a mohawk when she dried his hair because she couldn't get over how cute it was.
The goal was for him to be able to go 24 hours without needing oxygen assistance, and we were almost there. Once that happened he could spend the night in the room with us, while still be monitored every so often by the NICU staff popping in. Then we could take him home.
The only trouble was, I was at the end of my stay. It was discharge day and he wasn't quite ready to be taken off the oxygen yet. I was crushed. I couldn't leave my baby there and be so far away from him. The nurses rallied for us, and because he was doing so well, and my supply was up so we were able to supplement the donor milk with my own, we were able to stay in our room. When I started expressing I was getting maybe 1/8 of that tiniest syringe filled. By the time we were getting ready to check out I had graduated to putting it in the bottle! It doesn't seem like much, but it felt like a huge accomplishment.

The next morning we got great news when we went to see Judah; he was ready to come off the machines! They'd monitor his stats for a few hours and then he'd be released to come to our room for 24 hours of monitoring. Before they released him to our room they wanted to run one more set of tests - chest x-ray and ultrasound to check his lungs, labs to insure there was still no infection etc. And that's when there was {another} plot twist.
I know they can't help it, but when the nurses approach you with their eyebrows wrinkled up and their hands clasped together, you can always tell it's not good news. "We don't want you to panic," she started," but when we were doing his last set of tests, we found that Judah has a tiny hole in his heart."
I felt like I was caught in a rip tide; swirled around under the powerful force of the salty water, completely disoriented and unable to breathe.
Before I spun completely out of control, the doctor came over to explain things. It's called a ventricular septal defect, VSD for short, and is a somewhat common heart defect, especially in premature babies, that will usually close on its own. He would still be able to come to our room with us and go home in 24 hours if his stats remained steady, but it was something we'd need to follow up with in one month with a pediatric cardiologist. They reassured us we had nothing to worry about and that it would likely resolve on its own.
We wheeled back to our room as Judah dozed off, ready to start the two hour clock again, but this time with a packet in my lap that explained VSD with pictures and layman's terms.

As the two hours come to a close we started getting ready to walk to the NICU when there was a knock on the door, and in wheels our sweet boy in his basinet - completely wire- and tube-free! First order of business: cuddles. That night with him alone in our room I didn't sleep much. It was hard fighting the anxiety that he couldn't breathe and flashing back to our very first night together when he was grunting in effort to breathe while he slept. We made it through, and he woke up as the sky was painted in a beautiful sunrise and the room was filled with pinks and purples... and a fresh dose of hope. Today we would be going home.
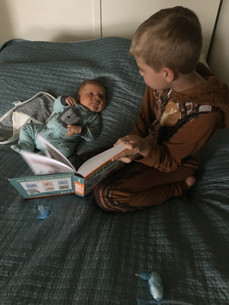
Our little Bird had pulled through. Our miracle of miracles. He'd lost a good amount of weight and was down to only 8lbs 4oz, was a bit jaundiced, and had a tiny hole in his heart - but to us he was perfection. God's promise fulfilled. And Big Brother, the one who prayed our little Judah into existence, was overjoyed to meet him. I don't think the smile on his face could have gotten any bigger. His joy was palpable and so sweet to witness.

* * *
A month later we discovered Judah's VSD had not closed on its own. And, in fact, there was another tiny hole in the upper chambers of his heart as well. Known as an Atrial Septal Defect (ASD), the tiny hole will likely cause no symptoms or problems, and may well close up into early childhood years. The cardiologist thoroughly examined the VSD as well, and was confident that it would not cause any issues and could still close on its own. It is something that is good to know about, and keep an eye on, but nothing to worry about. His next cardiology check up will be when he's one year old, and then again at five years old.
** Side Note: When I sent Bill the pic in the middle (he wasn't allowed in the appointment because of covid-19), he replied "Did you notice the elephant picture?" I hadn't noticed it, and he pointed it out because elephants have been popping up everywhere around this pregnancy and birth. Owen picked out the elephant lovey for him before he was born. A friend gave us her pack and play (from 10+ years ago when her kids were little) and there are elephants hanging from the toy bar. Another friend gifted us with clothes with elephants on them. Another friend gifted us a stuffed elephant that plays music. A gift bag at the baby shower had an elephant on it. A couple of the cards we got had elephants on them. They've been everywhere! We love that it's a reminder of God's promise as we prepare to return to Africa, but also of quiet strength - something the elephant so often symbolizes.
Now, at eleven weeks old (I know, it's taken me ages to finish this birth story!) our little Judah Phoenix is a big, happy, miracle. At his two month check up he was nearly 15lbs, he's wearing 3-6 month clothes and only waking (usually) two times a night to eat. He loves the outdoors, his big brother, cuddles, and being naked and/or in the bath.









































Comments